High Intensity Focused Ultrasound Helps Control Pain in Cancer Patients
Monday, Nov. 28, 2016
MR-guided high intensity focused ultrasound (MRgFUS) is a safe and effective method for managing pain in cancer patients and reducing their dependence on opioid medications, according to research presented Sunday by Alessandro Napoli, MD.
Pain affects up to 80 percent of cancer patients and has a strongly negative impact on quality of life and survival. Opioid pain medications are often prescribed for pain relief, especially in patients with advanced disease, but they have risks, including dependency. Other options like chemotherapy, radiation therapy and ablation carry their own set of risks and side effects.
Presenters Hans Peter Erasmus (left) and Alessandro Napoli, MD, presented research on pain management in cancer care.
Dr. Napoli said MRgFUS offers many benefits over those other options.
"This is a completely non-invasive therapy with no risk for bleeding or infection," said Dr. Napoli, a researcher in the Radiology, Oncology and Pathology Department at Sapienza University in Rome, Italy. "In addition, it's a highly precise technology, thanks to MRI real-time visualization and guidance that increases both the safety and the efficacy profile. Plus it is radiation free so there are no toxicity-related effects."
MRgFUS has emerged in recent years as an innovative and noninvasive alternative pain treatment for cancer patients. In the procedure, a transducer focuses ultrasound beams to induce an increase in temperature in the targeted area, destroying the tissue. Real-time monitoring with ultrasound or MRI increases the procedure's safety and efficacy.
MRgFUS has been studied to relieve pain in pancreatic cancer, bone metastases and recurrent cervical carcinoma. Dr. Napoli's group reported promising results in the management of patients with pancreatic cancer, a condition in which pain is notoriously difficult to control.
"This population of patients often has a poor prognosis and low life expectancy," said Susan Dababou, the study's lead author and a medical student at Sapienza. "The cancer-specific therapy is often very debilitating and pain can be a worsening factor of the general condition of these patients."
Studies showed that almost 80 percent of pancreatic cancer patients reported pain relief after focused ultrasound treatment. In one case described by Dr. Napoli, a 74-year-old female with stage III pancreatic cancer experienced significant pain reduction after MRgFUS ablation of a mass in her abdomen. Post-procedural MRI showed that important vascular structures near the treatment area were undamaged. The patient was able to stop daily consumption of opioid medications only two days after the procedure.
Promising results for MRgFUS have also been seen in patients who experienced cancer spread to their bones. An international multicenter study that included the Sapienza University researchers found pain palliation in more than 70 percent of patients with bone metastases. The technique has also shown promise in patients with recurrent cervical cancer, although more research is needed.
The duration of pain palliation, which is linked to the size of ablation of the tumor mass, can be substantial in the absence of disease recurrence, according to Dababou.
"The patients with pancreatic cancer treated with focalized ultrasound energy by our group were followed for six months and the pain relief lasted for the whole period," she said. "There is evidence of at least nine months of pain relief in bone metastases treated with MRgFUS."
Recent studies have shown that high-intensity focused ultrasound also has promising effects when coupled with chemotherapy and radiation therapy, improving patients' responses to anti-cancer therapy.
"In comparison with pharmacological treatment, MRgFUS acts on different fronts, ensuring an adequate pain relief, boosting the effect of chemotherapy and radiotherapy, and easing recovery," Dababou said. "The compliance of the patients is favored by the noninvasiveness and non-toxicity of the procedure, and unlike pharmacologic therapy it is a single session treatment with mild or no complications."
Presently, the main limitations of MRgFUS are cost and that not all parts of the body are accessible.
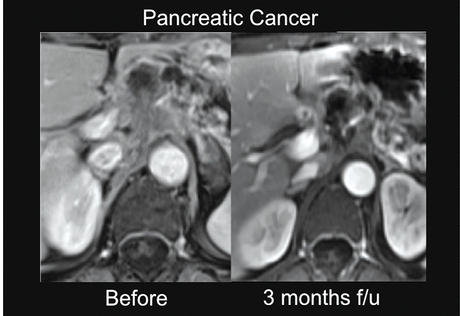
Axial contrast-enhanced MR image before treatment (left) shows the presence of pathological tissue within the pancreatic body determining encasement of the vascular celiac structures. Axial contrast-enhanced MR image three months after treatment (right) with non-perfused area corresponding to the ablated tissue, the surrounding vascular structures are preserved.
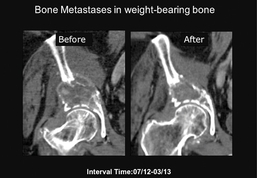
Coronal CT image acquired before treatment (left) shows a lytic lesion located in the right iliac bone with evidence of cortical erosion. Bone destruction reaches the acetabulum without articular invasion. Coronal CT image obtained eight months after treatment (right) demonstrates areas of de novo mineralization within the treated area and partial restoration of cortical bone.


 Home
Home Program
Program Exhibitors
Exhibitors My Meeting
My Meeting
 Virtual
Virtual Digital Posters
Digital Posters Case of Day
Case of Day